As wildfire season continues to affect vast regions across the United States and Canada, the dangers posed by wildfire smoke extend far beyond the immediate threat to our lungs. Recent research has revealed a startling connection between exposure to wildfire smoke and an increased risk of dementia – a connection that surpasses other forms of air pollution.
In a recent episode of “Austin on the Air,” our marketing director Stacy Malesiewski welcomed Dr. Anne Marie Fine, a leading expert in environmental medicine, to discuss these groundbreaking findings. Dr. Fine, co-founder and medical director of Environmental Medicine Education International, shared her insights into the study that has taken the medical community by storm.
The Alarming Link Between Wildfire Smoke and Dementia
The decade-long study Dr. Fine shared with the audience was recently presented at the Alzheimer’s Association International Conference (AAIC) 2024.1 It involved over 1.2 million people in southern California and has revealed that exposure to wildfire smoke significantly increases the risk of being diagnosed with dementia, more so than other types of air pollution. The research underscores the particularly hazardous nature of wildfire smoke on brain health.
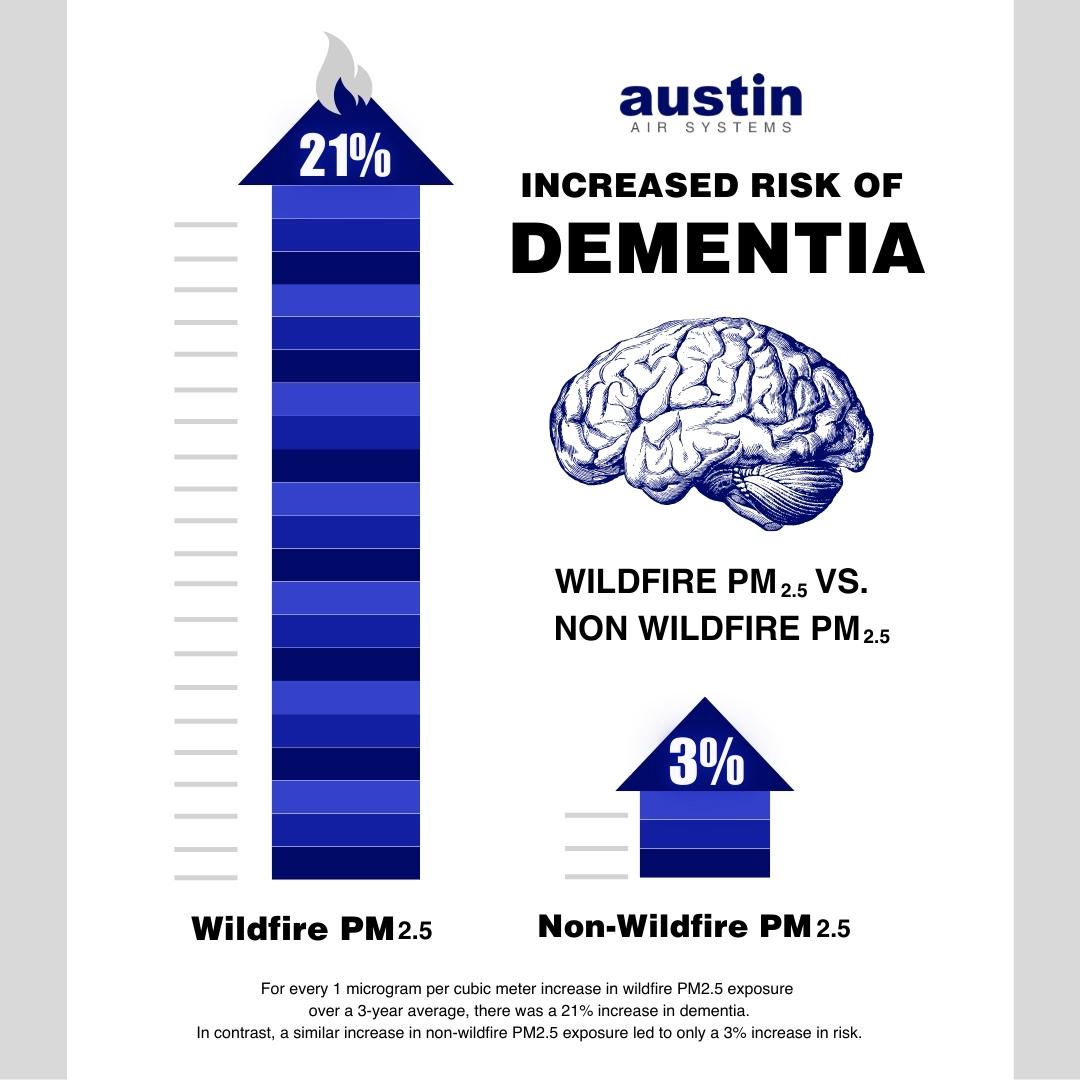
Wildfire smoke, along with emissions from motor vehicles and factories, contains fine particulate matter (PM2.5), a mixture of microscopic solid and liquid droplets. However, the study found that the risk of dementia diagnosis associated with wildfire PM2.5 exposure is notably stronger, even with lower exposure levels, compared to other sources of PM2.5.
The study’s findings suggest that wildfire smoke is more dangerous due to the higher temperatures at which it is produced, its greater concentration of toxic chemicals, and the smaller diameter of the particles compared to other PM2.5 sources.
For every 1 microgram per cubic meter (µg/m3) increase in wildfire PM2.5 exposure over a three-year average, there was a 21% increase in the odds of a dementia diagnosis. In contrast, a similar increase in non-wildfire PM<2.5 exposure led to only a 3% increase in risk. The effects were most pronounced in racially and ethnically minoritized groups and individuals living in high-poverty areas, highlighting the need for targeted health policies to address these disparities.
Given the rising incidence of wildfires, particularly in California and the western U.S., the study emphasizes the importance of updating home air filtration systems, staying indoors during poor air quality days, and wearing N95 masks when the Air Quality Index (AQI) exceeds 100. The findings point to a growing public health concern and the need for policies to prevent wildfires and mitigate their impact on brain health.
Dr. Fine emphasized that this isn’t just about respiratory issues. “We often think of wildfire smoke as primarily a respiratory issue because we’re breathing it in,” she explained. “But once it enters the body, it crosses the blood-brain barrier and impacts the brain in profound ways.”
Why Wildfire Smoke Is More Dangerous Than Diesel Exhaust
One of the key distinctions Dr. Fine made was between the particulate matter found in wildfire smoke and that found in diesel exhaust. While both contain harmful PM2.5, wildfire smoke is more concentrated and carries additional toxins like mercury and formaldehyde. These ultra-fine particles are small enough to enter the bloodstream, where they can travel to the brain, causing neuroinflammation—a driving factor behind neurodegenerative diseases like Alzheimer’s and Parkinson’s.
The Broader Implications: Indoor Air Pollution and Long-Term Health
The discussion didn’t stop at wildfire smoke. Dr. Fine also highlighted the pervasive issue of indoor air pollution. From off-gassing furniture and paints to gas stoves and air fresheners, our homes can be a source of continuous exposure to harmful chemicals. The Environmental Protection Agency (EPA) acknowledges that indoor air is often more polluted than outdoor air, making air filtration systems essential for maintaining a healthy living environment.
“Twenty-four years ago, I only recommended air filters for patients with asthma or COPD,” Dr. Fine shared. “Now, I see it as a necessity for everyone, given the myriad of pollutants we encounter daily.”
Dr. Fine also shared information about a variety of other interesting studies about brain and respiratory health, including the famous “Nun Study.”
Proactive Steps for Protecting Your Health
As the connection between environmental toxins and cognitive decline becomes clearer, the need for proactive measures is more urgent than ever. Dr. Fine stressed the importance of addressing these issues early, even before symptoms of diseases like Alzheimer’s manifest. Simple steps, such as improving indoor air quality with high-efficiency air filtration systems like the Austin Air HealthMate Plus, can make a significant difference in long-term health outcomes.
The study’s findings serve as a wake-up call. Wildfire smoke is not just an environmental issue—it’s a public health crisis that demands attention. By understanding the risks and taking preventive measures, we can protect ourselves and our loved ones from the long-term effects of air pollution.
For more information on environmental toxins and how to protect your health, explore resources at Environmental Medicine Education International. The new course “How to Thrive in a Toxic World,” is available to anyone, providing an opportunity to learn how to protect yourself.
To ensure the best defense against harmful air pollutants, consider investing in the Austin Air HealthMate Plus. Featuring a special blend of activated carbon impregnated with potassium-iodide, it is specially crafted to adsorb smoke, toxins, gasses, and VOCs.
REFERENCE
1 Alzheimer’s Association. (2024 July 29). Exposure To Wildfire Smoke Greatly Raises Risk Of Dementia Diagnosis. [Press release.] https://aaic.alz.org/downloads2024/AAIC-2024-Wildfire-smoke.pdf.